When love literally hurts: endometriosis and painful sex
Sex. Intercourse. Making love. F*cking.
Whatever you call it, there’s no denying sex is a fundamental part of the human experience.
But for people with endometriosis, sex can be an uncomfortable, if not outright painful experience.
Looking back, pain during sex was one of the very first endometriosis symptoms I experienced. When I had sex for the first time at 16 it was so painful I cried, but we were taught in school that it was normal for it to hurt when you lose your virginity.
My friends assured me that their first time hurt too, and that it would get better.
But for me, the pain never went away. I just learned to ignore it, and secretly wondered if everyone else was lying about sex being so much fun.
It took me nearly ten years after that first time to be diagnosed with endometriosis, and while pain during intercourse became the least of my worries symptom-wise, it has had a very significant impact on both my romantic relationships and self-worth over the years.

After two surgeries, various hormone treatments and other medications, pelvic floor physiotherapy and a lot of actual therapy, at 25 years old I’m now able to enjoy relatively pain-free sex most of the time.
I wish I could tell that 16 year old girl that she doesn’t have to suffer in silence.
But I can’t, so I’m hoping this will reach someone who needs to hear it.
What is endometriosis? endometriosis?
Endometriosis is a condition where tissue similar to the lining of the uterus (the endometrium) is found outside the uterus, i.e. on other organs. This causes a chronic inflammatory reaction in the body that may result in scar tissue.
It is estimated to affect 1 in 10 people assigned female at birth, which equates to around 120,000 people in New Zealand and almost 200 million worldwide.
Symptoms can include painful periods, painful ovulation, bowel related problems like IBS, chronic pelvic pain, fatigue, sub-fertility and pain during or after sexual intercourse.
There is currently no cure for endometriosis.
Endometriosis and painfulpainful sex
The World Endometriosis Foundation reports that 42% of people with dyspareunia have avoided intercourse altogether because of pain, or the lived experience of associated pain, leading to anxiety or fear with sexual activity.
Tanya Cooke, CEO at Endometriosis New Zealand (ENZ), says dyspareunia and its impacts can affect your physical and psychological well-being, body image, self-esteem, confidence and relationships.
“When you have endometriosis, sex can be painful. That pain, coupled with the anticipatory fear of pain, can turn you off intimacy big time. Those with endometriosis often feel like their own body has let them down.
“Feelings of disappointment, fear, guilt, inadequacy and shame can become the norm from the first sexual encounter, and overcoming these experiences requires understanding, expertise from your health team and self-management,” she says.
People with endometriosis who experience dyspareunia have described it as sharp, stabbing, jabbing or a deep ache. It can be mild or excruciating, and may be felt during intercourse, or for up to 24-48 hours after intercourse, or both.
Some endometriosis sufferers experience pain with any form of intercourse, while others experience it only with deep penetration. Some feel pain only at certain times of the month, such as during their period, while others feel it throughout the month or randomly, like in certain sex positions.
Why does endometriosisendometriosis cause painful sex?
According to ENZ, there’s no straightforward answer to this.
“Despite pain during sex being a common symptom of endometriosis, the reasons why can be varied and complex. Endometriosis is now described as an inflammatory disease, and excessive inflammation in endometriosis contributes to changes of hormonal regulation by changing sex steroid receptors.
“Painful pelvic muscles can become tight, which can also contribute to painful sex. There are other theories and further research is underway to improve our understanding of this often debilitating symptom. The studies usually conclude that more research is needed,” says Cooke.
What can II do about it?
Currently, laparoscopic excision surgery is often the recommended treatment for endometriosis, and can bring relief from many symptoms including dyspareunia.
“However, increasingly, we know that surgery is not the only answer to relieve the symptoms of endometriosis including dyspareunia, particularly if this has been distressing for a while and has caused fear and anxiety,” says Cooke.
Laparoscopic surgery is sometimes combined with the placement of an IUD, which many people with endometriosis report they find effective in managing symptoms long term. Other forms of birth control or hormonal medications can also ease symptoms, and some surgeons believe that nerve block injections can be helpful in minimising the pain from nerves which have become irritated.
ENZ recommends a multidisciplinary approach, particularly if pain persists despite surgical excision.
“Sexual functioning is a complex, multidimensional phenomenon, and so ideally the treatment for endometriosis-related sexual dysfunctions should be conducted by a multidisciplinary team.
“This could include pelvic floor physiotherapy, exercise, seeing a dietician, and also psychological treatment to help not only with pain management, but also the anxiety and relationship impacts that come with painful sex.
“The impacts of endometriosis on peoples’ sex lives requires more research, not only on pain during intercourse but on the psychological and relationship aspects too,” she says.
Just because painful sex is common, doesn’t mean you have to accept it as “normal”. While occasional, minor soreness is probably nothing to worry about, if you are having intense or frequent pain please talk to your GP and know that you are not alone, and you are not broken.
For more information about endometriosis, visit nzendo.org.nz


Related Posts
Kiwis turn to books for self-love this Valentine’s Day
Kiwis are more dedicated to self-love this Valentines Day
Swings, candles, games and bondage: Everything you need when creating your own sex room
Get ready to make your 50 shades fantasy a home reality
Celebrating International Women’s Day: Natasha Neal
Celebrating International Women's Day with Natasha Neal
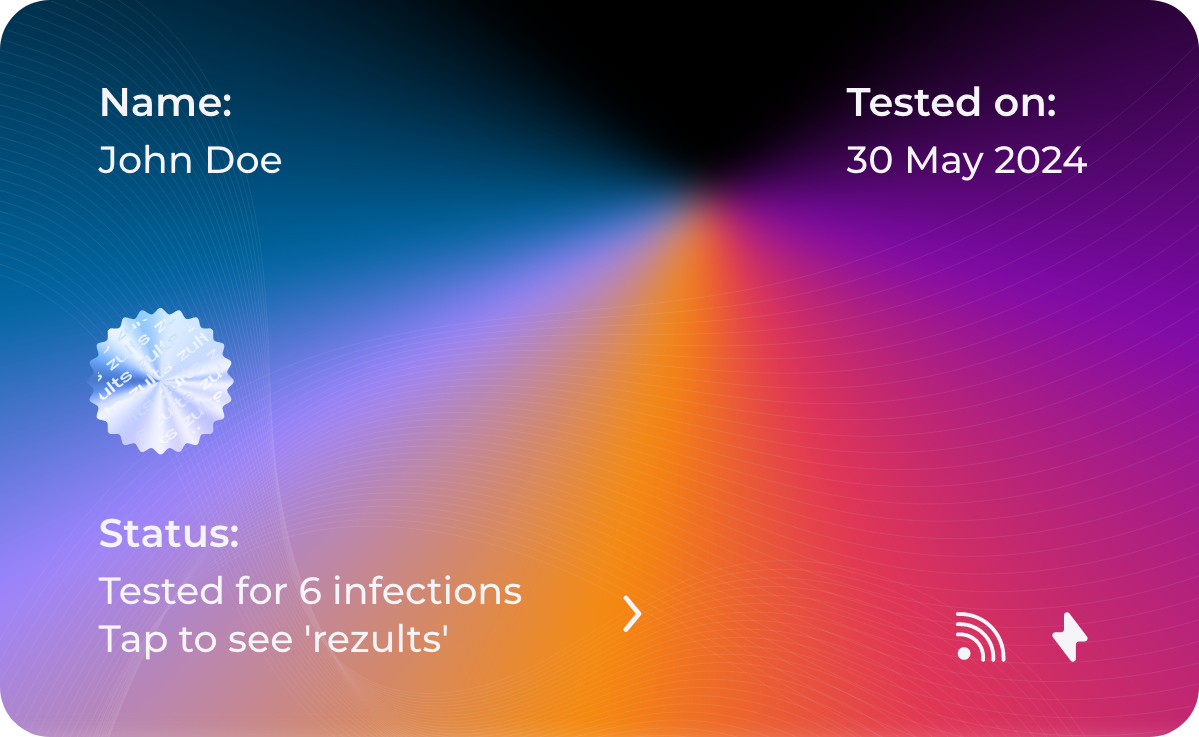
Zults: Revolutionising Sexual Health Conversations in the UK
A new technology, Zults, has launched in the market and is designed to transform the way we share and discuss STI results. Developed in collaboration with Sexual Health London (SHL), Zults offers a platform that enables users to manage and share thei
Kama’s ‘Mother of Orgasms’ talks pleasure, sex and market domination
An interview with Taslim Parsons, the 'Mother of Orgams'
85 years young: Family Planning survey shows sexual health clinics are more important than ever
The experts at Family Planning speak to Nak-Ed on their importance